Six in 10 professionals feel health system is unsafe for homeless and excluded people
Six in 10 health professionals feel the health system is unsafe for people facing homelessness and other forms of social exclusion, a survey has found.

A report from Pathway and Crisis, the charities, revealed that following the NHS definition of patient safety as “the avoidance of unintended or unexpected harm to people during the provision of healthcare”, 60% of survey respondents felt that the health system was unsafe for people in inclusion health groups and 11% felt it was safe.
The survey involved 180 staff across England working in the health, housing, social care and third sector to examine how people in ‘inclusion health’ groups struggle to access health services.
Inclusion health describes people who are socially excluded, such as people who are experiencing homelessness, sex workers, vulnerable migrants, Travellers and those in the criminal justice system.
Survey respondents said that people in inclusion health groups are commonly discharged to the street (58% all the time or often), to unsuitable temporary accommodation (71%) and with unmet health needs (79%).
The inability of the housing system to provide a safe place to recover after hospital admission is central to the “revolving door” in secondary care, an expensive and inefficient way of delivering healthcare, the report said.
Urgent and emergency care is the most accessible, but even here just 31% of professionals said it was easy to access, with 45% seeing it as difficult or very difficult to access.
Other services such as mental health (92% difficult or very difficult), dentistry (87%) and general practice (69%) were even harder for excluded groups to access.
Nearly half of survey respondents reported seeing improvements in collaborative working between health, housing and social care, while 40% saw an improvement in trauma-informed care.
However, 40% of professionals felt that health outcomes for people in inclusion health groups would worsen over the next three years, 32% said they would stay the same and just 20% that they would improve.
Pressure on the NHS, issues around adequate funding for services and integration, and the housing crisis were highlighted as key barriers to improvement.
A third of survey respondents reported seeing improvements in training and education relevant to inclusion health over the past year, while 40% reported improvements in trauma-informed care.
However, the report found there are still large training gaps. Fewer than half (42%) of staff members working in mainstream health services felt that they had enough training to effectively support people in inclusion health groups, along with 63% of those working in specialist services.
The report said the government’s proposed ‘shifts’ for the NHS – from analogue to digital, hospitals to community and sickness to prevention – can benefit people in inclusion health groups, but “run the risk of further excluding them if their specific needs and circumstances are not considered”.
Survey respondents were positive about the possible impact of shifting care from hospitals to the community: 57% thought this would have a positive impact for inclusion health groups and 68% thought shifting from sickness to prevention would.
In contrast, 61% of professionals felt the shift from an analogue to a more digital NHS would have a negative impact on people in inclusion health groups.
The report noted that improvements in the availability of basic housing must be accompanied by improved provision of specialist and supported types of accommodation, such as Housing First and care homes for younger people.
It recommended that the government should scale up intermediate care services, encourage general practice to provide longer, more flexible appointments, capture patients’ housing status in NHS data, align the homelessness strategy with the forthcoming long-term housing strategy and establish a national inclusion health workforce programme.
The report came after Paula Barker, co-chair of the All-Party Parliamentary Group for Ending Homelessness, wrote to Wes Streeting, the health secretary, and Angela Rayner, the housing secretary, urging them to address health inequalities facing homeless people.
In the letter, dated 11 March, Ms Barker said an admission to hospital was an opportunity to intervene to end someone’s homelessness, but “too often this opportunity is missed”, with patients facing homelessness continuing to be discharged onto the street.
She cited a recent Freedom of Information request which found that at least 4,200 people were discharged from hospital without a safe place to recover in 2022-23, “perpetuating the cycle of readmissions and putting pressure on the NHS”.
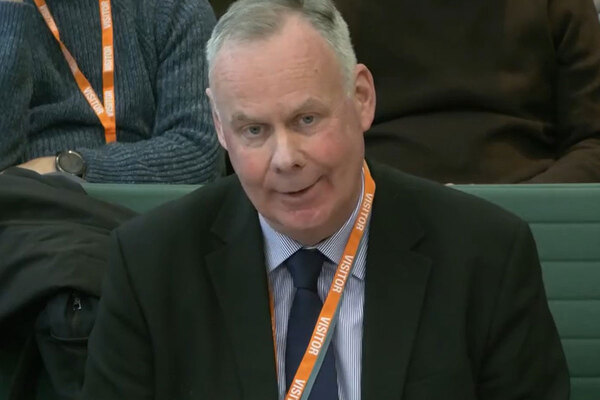
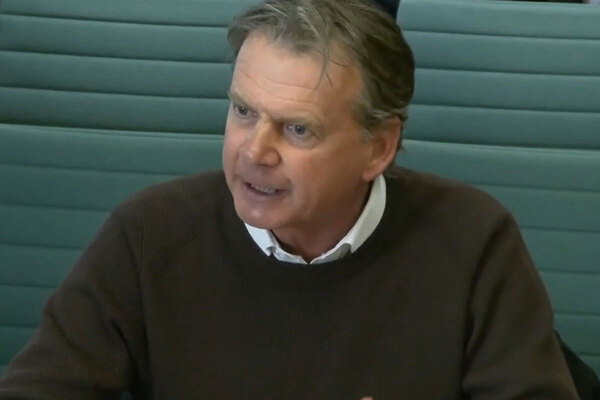
Alex Bax, chief executive of Pathway, and Matt Downie, chief executive of Crisis, said: “For the government to realise its stated goals – shifting care to the community and investing more in prevention – for people facing social exclusion, we need to see sustained investment in the provision of specialist inclusion health hospital, primary care and step-down services, along with reforms to make mainstream services more accessible and welcoming.
“These improvements in care must happen alongside a step-change in the provision of safe, good-quality, genuinely affordable homes. Building the 90,000 social rented homes per year that we need will make a huge contribution to the population’s health.”
The Ministry of Housing, Communities and Local Government and the Department of Health and Social Care were approached for comment on the report.
Sign up for our homelessness bulletin
Already have an account? Click here to manage your newsletters