You are viewing 1 of your 1 free articles
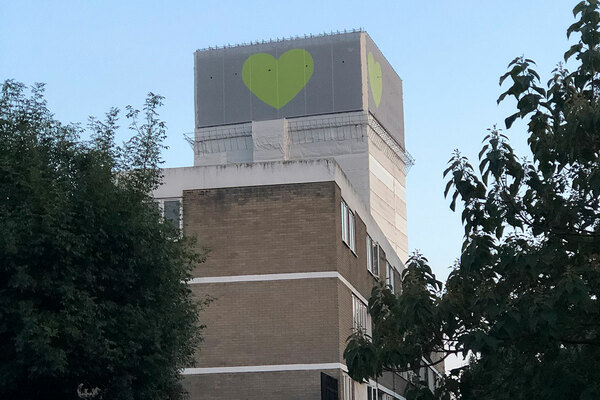
Homeless people are being refused healthcare access, report finds
Homeless people face some of the worst access to healthcare due to discrimination and stigma, a report has found.
Homelessness charities Crisis and Pathway said the country’s health and housing systems were both facing a crisis, with the average age of death for homeless men just 46 and only 42 for women.
The report, Always at the bottom of the pile, surveyed 156 medical professionals across England to examine how people in ‘inclusion health’ groups struggle to access health services.
Inclusion health describes people who are socially excluded, such as people who are homeless, drug and alcohol dependent, vulnerable migrants, travellers, sex workers and victims of modern slavery.
According to the charities, two-thirds of healthcare professionals reported that people without proof of address or ID were refused access to GP services.
In addition, three-quarters of healthcare professionals said that homeless people were often or always discharged from hospital to the street with unmet health needs.
Such exclusion leads to preventable diseases being left untreated, the report said, resulting in health deteriorating and premature death. It also meant people have to wait until their condition worsens to get support, leading them to rely on costly services such as A&E and urgent care.
Fewer than one in five people who use substances alongside experiencing mental health problems receive appropriate support for both conditions, the report said. This is a particular problem given that many homeless people ‘self medicate’ with drugs and alcohol.
Dentist services for people in inclusion health groups were described as “non-existent” by respondents. According to homeless health needs assessments, just over half of homeless people were registered with a dentist, compared with 80% of the general population.
“There is clear evidence that inclusion health groups face stigma and discrimination in health service contexts,” the report added.
Pathway and Crisis have called on the government to increase the availability of specialist care and deliver more social homes to ensure no one was shut out from the healthcare system.
Two-thirds of professionals surveyed cited lack of resources as a barrier to providing effective care, with 59% describing uncertainty of funding as a challenge.
The charities recommend that a national ‘safe discharge’ programme is established to end the unsafe practice of discharging patients from hospital to the street.
Alex Bax, chief executive of Pathway, said: “[The report] paints a bleak picture of overstretched, inflexible services leaving people to wait until they are at crisis point before they get any care. This is obviously bad for individuals and bad for the NHS – prevention and earlier intervention would be cheaper and better all round.”
He added that the government “must make clear its expectations that NHS services should be more accessible to people who are socially excluded and end dangerous practices such as discharge from hospital to the streets”.
Matt Downie, chief executive of Crisis, said thousands of homeless people are being “pushed away” from healthcare services due to “something as simple as lack of address or ID”, meaning health issues are often left untreated until they get to a critical point.
He added: “We also desperately need a long-term plan to increase housing supply, starting by building the 90,000 social homes a year we need to end homelessness for good.”
Sign up for our homelessness bulletin
Already have an account? Click here to manage your newsletters